Doctors' stories.
Spoken, written and heard.
The year I started medical school, we were the first class to be half female.
A glossy magazine wrote a feature article about us, this curious phenomenon, the female doctor. Alongside the article was a photograph of young female model, dressed in surgical scrubs with heavy make-up. The title of the article was, Would you trust this woman with your life?
Amazingly, in 1983, that seemed a reasonable question.
We didn’t have a female doctor teach us until my fourth year.
It was hard to work out how to be me, a female, a mother and be a doctor. ‘Good’ GPs did 60 hour weeks, 100 births a year and were constantly available after hours. It seemed to be a job description that required a ‘wife’.
We were told we were the cream of the crop on day one. I found the statement at best cringe-worthy, at worst a statement oozing power without humility.

Medicine is a fantastic tool, but illness is told through the medium of story.
I have spent my career intrigued by the culture of medicine, the disconnect between the intent to help people and the reality of the harm we can do to people just by the way we are. The medicine we learnt was great but the rest was really a training in how not to be a doctor. Occasionally we saw a remarkable physician in action, speaking to patients with humanity and kindness but that was pretty unusual.
In the end the patients taught me most. But I had to listen, not just to their words but to their stories… Stories that get told in whispers, in baffling behaviours and in bodies.
I hope always to feel my way into a conversation in which the patient can discuss what really matters and leave the room feeling a little better than when they came in. It’s one of those aspirational destinations, we don’t always get to, because we are human too.
Mentors helped my story. Sometimes you have to seek them out, be brave, ask for a conversation. Wise mentors have helped me to understand my assumptions and change my thinking. They challenged me to create some other way of being my doctor self.
Burnout was a huge experience for me.
My burnout was a result of too much ‘life’ on top of my job. If anything, sitting with patient’s stories is what nourished me and in my recovery all the stories I had heard helped me make sense of my own story. But burnout came with a profound sense of shame and failure at not reaching the standard of the real doctor. In medicine one of the worst crimes is not to cope or not to know.
What I have realized that the expectations that we should cope under insurmountable pressure is the thing that is not reasonable. It has been a great liberation to free myself from shame.
Writing helps. Putting these things on the page has helped my see them without the imagined commentary.
I have written detailed account of my burnout story in my book and shared it ‘shamelessly’ on many occasions! In sharing my story I have learnt how common these stories are for doctors and how seldom they are spoken of. If me speaking allows you to speak that would be a great thing.
Nowadays I put burnout on my CV and can honestly say my life has been enriched. I wouldn’t want to go back.

Narrating our selves
Eric Elder lecture, RNZCGP Conference, Auckland, 2016.
An exploration of how doctors create their identity through the stories they observe or take part in
Interviews
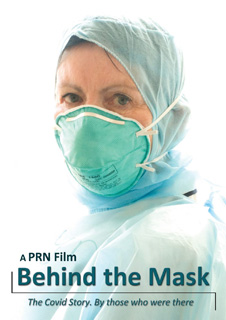
Paul Trotman, interviewed me in May 2020 whilst researching for his documentary ‘Behind the Mask’.
The interview is a really interesting conversation about how life was in the first few months of the pandemic.
The final documentary by Paul Trotman is incredible. Read my review of ‘Behind the Mask’ here.
The film is available on Vimeo. It is a gripping reminder.

Interview on NZ General Practice Podcast with the lovely Dr Jo Scott-Jones. Recorded April 2020 early in the Covid19 pandemic.
